Congestive Heart Failure (CHF)
Congestive heart failure is a long-term condition in which heart can not pump blood well enough to provide normal supply to body. Due to reduced cardiac output, body cannot perform its normal metabolic needs. The reduced supply of oxygen and nutrients may lead to inadequate tissue perfusion, vascular, cardiac and pulmonary congestion. This cardiac and pulmonary congestion is collectively known as the congestive heart failure. Blood and fluids accumulate in heart, lungs and legs.
The term heart failure means failure to function as efficient pump and not total stoppage of heart. In this case heart is in working condition but it is unable to handle normal blood supply.
Etiology
Any factor which affects the heart and interferes with the normal blood circulation can cause heart failure. These factors can affect cardiac output either singly or in combination. Most commonly observed factors and diseases are given below.
- Impaired filling of heart chambers: Some diseases limit the full relaxation of heart and hence heart chambers unable to get fill properly. Example of such disease is pericarditis and pericardial stiffness.
- Increased workload on the heart: The increased work load is of two types, pressure load and volume load. Some conditions like systemic and pulmonary hypertension, chronic lung disease may increase pressure load. On the other hand, heart valve diseases or overactive thyroid gland may increase volume load. This pressure or volume load initially results in enlargement of fibres and produces stronger contraction. But as the enlargement increases the pumping ability of heart decreases.
- Intrinsic pump failure: The heart wall (myocardium) has intrinsic capacity to contract and relax on its own to work as a pump.
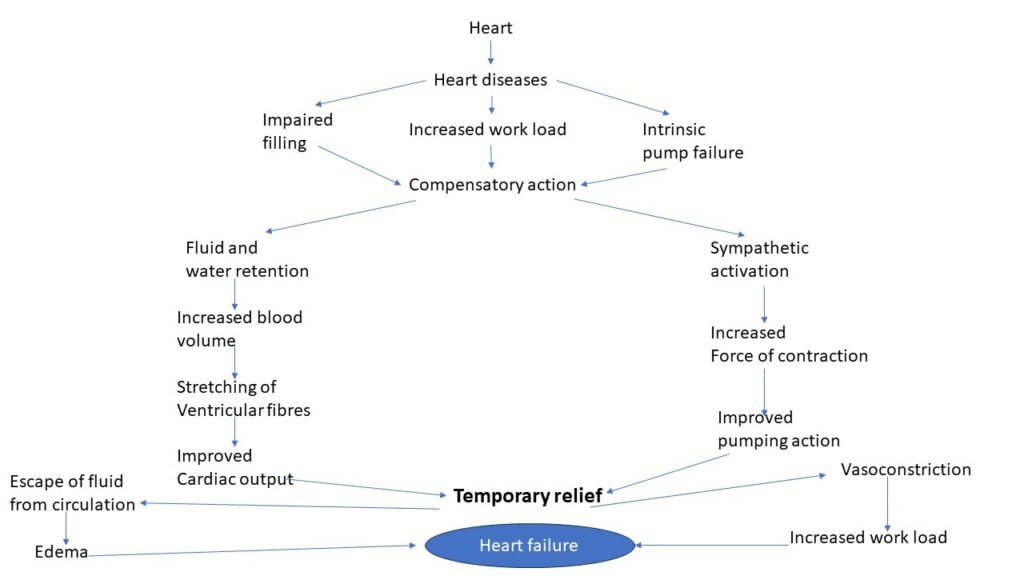
Pathophysiology
There are three primary compensatory mechanisms to maintain normal cardiac function. These mechanisms attempt to maintain cardiac function which is reserved for the time of cardiovascular stress and exercise.

When these compensatory mechanisms become insufficient or active for a long period, they become ineffective and results in heart failure. The decrease in cardiac output increases the pulmonary capillary pressure above the critical level (25-40mm of Hg). Due to high pressure fluid escapes from capillaries and accumulates in interstitial spaces. This accumulated fluid interferes with gaseous exchange and leads to pulmonary congestion associated with breathlessness.
Types of heart failure
Types of heart failure are given in table below.
| Type | Description |
| Acute heart failure | It is a sudden and rapid development of failure followed by myocardial infarction, valve rupture, myocarditis, etc. prominent features are sudden reduction in cardiac output and hypotension without edema. |
| Chronic heart failure | Develops slowly with gradual reduction in cardiac output. Blood pressure is well maintained but associated with peripheral edema. Commonly observed in systemic arterial hypertension, chronic obstructive pulmonary disease. |
| Left sided heart failure | Happens due to accumulation of fluid upstream in the lungs and results in stress to the left side of heart. Common clinical manifestations are pulmonary congestion, edema, hypoperfusion, dyspnoea, etc. |
| Right sided heart failure | Generally, occurs after left sided heart failure and affects the right side of heart. Common clinical manifestations are systemic and portal congestion, reduced cardiac output, congestive hepatomegaly, etc. |
| Forward heart failure | In this case cardiac output is decreased leading to hypoperfusion especially renal perfusion. The renal hypoperfusion results in sodium and water retention (edema). |
| Backward heart failure | In this case ventricles fail to pump blood normally resulting elevated pressure and volume. Sodium and water retention is also observed associated with edema. |
| Systolic heart failure | Happens due to predominant systolic ventricular dysfunction, mainly due to myocardial dysfunction, ischemic heart disease, chronic excessive ventricular workload, etc. |
| Diastolic heart failure | Happens due to inadequate relaxation of ventricles leading to elevated pressure with normal ventricular volume. |
| High output failure | Here heart act as abnormal pump and has high output. Initially it gives well perfusion but eventually fails due to excessive oxygen demand. |
| Low output failure | In this case failure of pump with marked reduction in cardiac output is seen. |
Heart cell changes
During the process of heart failure, heart cell undergoes changes to prevent or postpone the heart failure. These changes are hypertrophy, dialation or both. This is well illustrated in below flow chart.
Cardiac failure (initial phase) –> Increase in overload/ pressure load/ both –> Increased cardiac work load –> Stretching followed by Elongation of ventricular fibres –> Compensatory hypertrophy and cardiac dilation –> Temporary compensation –> Failure to compensate –> Heart failure
Clinical manifestations
The signs of CHF are different with respect to predominant side involved. Some of the major clinical manifestations are described below.
- Various grades of dyspnoea: It is due to accumulation of fluid into interstitial and alveolar spaces. Reduced sympathetic tone, reduced sensitivity of respiratory centre and reduced blood pooling in the extremities during sleep are responsible for nocturnal dyspnoea and orthopnoea. In addition, distention of lungs leads to respiratory muscle fatigue.
- Fatigue: Reduced cardiac output and hypoperfusion of skeletal muscles are responsible for fatigue.
- Cerebral symptoms: Commonly seen cerebral symptoms are confusion, reduced concentration, headache, sleep disturbances and anxiety. This happens due to reduced cerebral blood flow.
- Chest pain: Reduced coronary blood supply leads to chest pain.
- Gastrointestinal symptoms: Congestion of gastric mucosa, liver and portal venous system result in nausea, loss of appetite, abdominal pain, etc.
- Nocturia and oliguria: During day time renal hypoperfusion results in sodium and water retention and in night comparatively improves perfusion causes nocturia called as night diuresis. These symptoms are predominantly seen in left sided heart failure.
- Edema: Decreased pumping activity of heart leads to swelling in feet, ankles, liver, abdomen, etc. the systemic venous congestion is important to produce generalized edema.
- Shortness of breath: Pulmonary edema causes shortness of breath. Initially it occurs upon exercise but later can be experienced even at rest.
- Right upper quadrant pain: Expansion of liver and ascites can lead to pain in right upper quadrant of the abdomen.
- Physical signs
- Fast and low volume pulse
- Elevated jugular venous pressure
- Pale, cold and sweaty skin (due to vasoconstriction)
- Pleural effusion (due to congestion)
- Third heart sound in adults (due to rapid flowing of ventricles)
- Appearance of fourth heart sound (due to rapid filling of ventricles)
Morphological consequences
- Hypertrophy (increased size and weight) followed by dialation.
- Formation of thrombi due to stagnation of blood.
- Large, heavy and deeply congested lungs.
- Thickening of alveolar septal walls.
- Overweight, congested and tender liver which may shrink on long standing venous congestion.
- Nutmeg appearance (alternate dark and pale areas) to the liver.
- Enlarged, congested and firm spleen with marked dialation and focal haemorrhage.
- Ischemic damage to other visceral area especially kidney, GIT and cerebral tissue may result in ulceration followed by gangrene.
Management of CHF
As there is no cure for heart failure, prevention is the best practice. Improving the lifestyle and good quality of life can help to avoid heart failure. Adequate rest and regular exercise may lead to improvement. Removal of contributing factors like excessive exertion, overweight, alcohol consumption and cigarette smoking is useful.
The management of heart failure has three important objectives as follows,
- Treatment of underlying causes
- Removal or avoidance of precipitating factors
- Actual treatment of heart failure (pharmacotherapy)
The ideal approach to treat the CHF is to treat the underlying cause like correction of narrowed valve, blocked coronary arteries, etc.
Pharmacotherapy
Ionotropic (increase in force of contraction) drugs: Digitalis glycosides show positive ionotropic effect (increases force of contraction) and negative chronotropic effect (decrease in heart rate). Digitalis inhibits the Na+ K+ ATPase and reduce Ca++ expulsion from the cells by Na+ Ca++ exchanger. The elevated intracellular Ca++ ion concentration in the vicinity of contractile proteins result in adequate force of contraction.
Sympathomimetic amines like dopamine and dobutamine are used in chronic cases of heart failure.
Phosphodiesterase enzyme inhibitors inactivates cAMP and cGMP showing increase in cardiac output, decreased vascular resistance via vasodilation.
Drugs without positive ionotropic effects
Diuretics: These drugs promote sodium and water excretion, hence reduces edema and preload on heart. Example of diuretics are torsemide, furosemide, spironolactone, etc.
Angiotensin converting enzyme inhibitors: These drugs reduce peripheral resistance and reduces afterload. They also reduce aldosterone secretion to retain salt and water. For example, enalapril, ramipril.
Vasodilators: Vasodilators are responsible for selective arterial vasodilation or venodialation or both.
Surgical treatment
Heart transplantation may be recommended for people who do not respond to medication.
For more regular updates you can visit our social media accounts,
Instagram: Follow us
Facebook: Follow us
WhatsApp: Join us
Telegram: Join us
