Blood
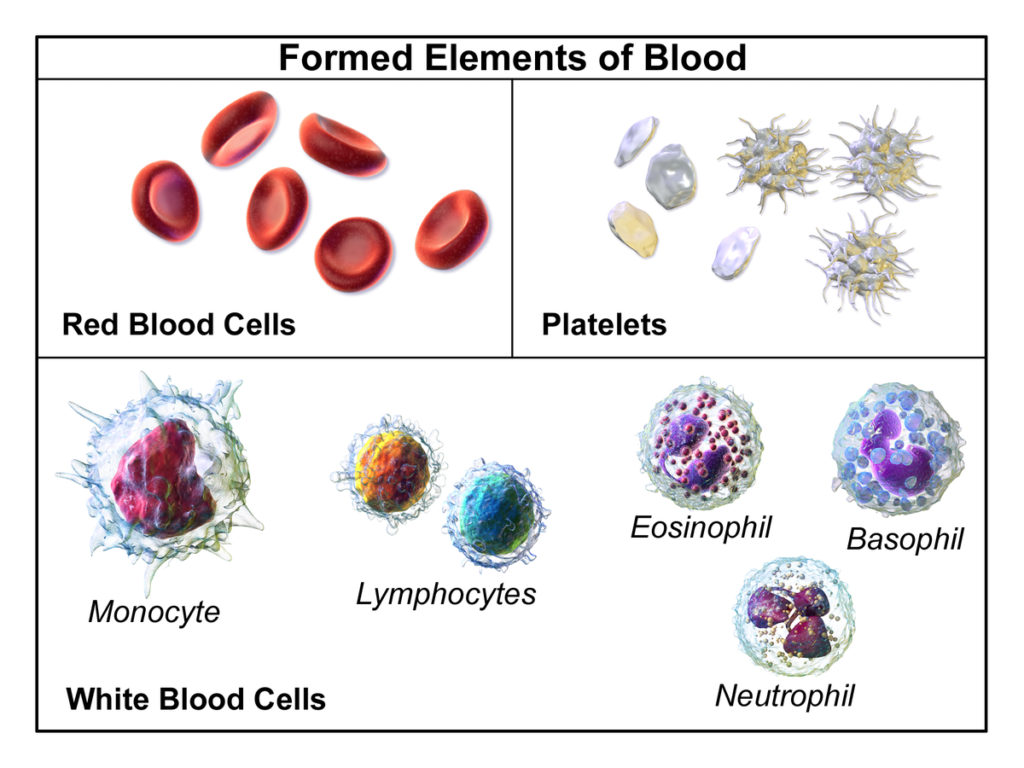
Blood, the life-sustaining fluid, is as vital to our existence as the air we breathe. It is a specialized form of connective tissue that courses through our veins and arteries, a silent river that nourishes every cell in our body. Composed of plasma, red blood cells, white blood cells, and platelets, blood performs a multitude of functions. It delivers essential nutrients and oxygen to our cells, removes metabolic waste, fights off infections, and even helps regulate our body temperature. This article aims to delve into the fascinating world of blood, exploring its composition, functions, circulation, and the disorders that can affect this vital fluid.
Composition of blood
Plasma (55% of total blood volume)
- Plasma is a yellowish fluid that is mostly water (92% by volume), but contains proteins, glucose, mineral ions, hormones, carbon dioxide (the waste product of respiration), and blood cells themselves.
- It serves as a transport medium for delivering nutrients to the cells of the various organs of the body and for transporting waste products derived from cellular metabolism to the kidneys, lungs, and liver for excretion.
Red Blood Cells (Erythrocytes)
- Red blood cells, or erythrocytes, are the most common type of blood cell and the vertebrate organism’s principal means of delivering oxygen to the body tissues via the blood flow through the circulatory system.
- They are filled with hemoglobin, a protein that binds oxygen and gives red blood cells their color.
- The shape of red blood cells is biconcave—disk-shaped, but depressed in the center on both sides.
White Blood Cells (Leukocytes)
- White blood cells, or leukocytes, are cells of the immune system involved in protecting the body against both infectious disease and foreign invaders.
- They are much fewer in number than red blood cells, accounting for about 1 percent of your blood.
- The two main types of leukocytes are granulocytes (neutrophils, eosinophils, and basophils) and agranulocytes (lymphocytes and monocytes).
Platelets (Thrombocytes)
- Platelets, or thrombocytes, are very small, irregularly shaped clear cell fragments, 2–3 µm in diameter, which derive from fragmentation of precursor megakaryocytes.
- The average lifespan of a platelet is normally just 5 to 9 days.
- Platelets play a fundamental role in hemostasis and are a natural source of growth factors. They circulate in the blood of mammals and are involved in hemostasis, leading to the formation of blood clots.
Functions of blood
Supply of Oxygen
Blood is responsible for transporting oxygen from the lungs to the various cells of the body. This is carried out by red blood cells, which contain a protein called hemoglobin that binds to oxygen.
Supply of Nutrients
Blood also transports nutrients such as glucose, amino acids, and fatty acids, which are absorbed from the food we eat, from the digestive tract and stored in the body to the cells.
Removal of Waste
Metabolic waste products such as carbon dioxide and urea are transported by the blood from the cells to the lungs, kidneys, and liver for excretion.
Immunological Functions
- White blood cells in the blood help protect the body against diseases. They identify and destroy pathogens and cancer cells.
- Antibodies in the blood help neutralize toxins produced by these pathogens.
Coagulation
- Blood has the ability to change from a liquid to a gel in order to plug leaks in blood vessels and prevent loss of blood. This process is known as coagulation.
- Platelets, a type of blood cell, along with proteins in the plasma, help form clots to seal wounds and prevent excessive bleeding.
Messenger Functions
- Blood carries hormones, which are chemical messengers, from the glands where they are produced to the organs they affect.
- It also carries signaling molecules like cytokines and chemokines, which help coordinate immune responses.
Regulation of Body Temperature
Blood helps regulate body temperature by redistributing heat. For example, when you’re exercising, blood flow to your skin increases to help cool your body.
Hydraulic Functions
Blood, being a fluid, is also responsible for hydraulic functions in the body. For example, the hydraulic pressure provided by blood flow or heartbeat maintains the erection of the penis in males.
Hemopoeisis
Hematopoiesis is the production of all cellular components of blood and blood plasma. It occurs within the hematopoietic system, which includes organs and tissues such as the bone marrow, liver, and spleen.
Hematopoietic Stem Cells (HSCs)
- Hematopoiesis begins with hematopoietic stem cells (HSCs) that reside in the bone marrow.
- These HSCs have the unique ability to give rise to all different mature blood cell types and tissues.
- HSCs are self-renewing cells: when they differentiate, at least some of their daughter cells remain as HSCs so the pool of stem cells is not depleted.
Cell Types
- Red blood cells (erythrocytes): These transport oxygen and hemoglobin throughout the body.
- White blood cells (leukocytes): These support the immune system. There are several different types of white blood cells.
- Platelets (thrombocytes): These help the blood to clot.
Hematopoiesis Location
- Hematopoiesis occurs in many places. It begins during the first weeks of embryonic development.
- In adults, hematopoiesis of red blood cells and platelets occurs primarily in the bone marrow.
- The lymph system, particularly the spleen, lymph nodes, and thymus, produces a type of white blood cell called lymphocytes.
- Tissue in the liver, spleen, lymph nodes and some other organs produce another type of white blood cells, called monocytes.
The Process of Hematopoiesis
Multipotent Hematopoietic Stem Cells (HSCs)
- Hematopoiesis begins with hematopoietic stem cells (HSCs) that reside in the bone marrow.
- These HSCs have the unique ability to give rise to all different mature blood cell types and tissues.
Commitment and Early Differentiation
- HSCs differentiate into two main progenitor cells: Myeloid and Lymphoid progenitors.
- Myeloid progenitors give rise to red blood cells, platelets, and certain types of white blood cells (neutrophils, eosinophils, basophils, and monocytes).
- Lymphoid progenitors give rise to other types of white blood cells, specifically lymphocytes.
Late Differentiation and Maturation
- The committed progenitors further differentiate and mature into functional blood cells.
- This process is guided by a myriad of growth factors and cytokines.
Regulation of Hematopoiesis
- The rate of hematopoiesis depends on the body’s needs.
- The body continually manufactures new blood cells to replace old ones.
- About 1 percent of the body’s blood cells must be replaced every day.
- White blood cells have the shortest life span, sometimes surviving just a few hours to a few days, while red blood cells can last up to 120 days.
Formation of hemoglobin
Hemoglobin Synthesis
Hemoglobin is synthesized together with the red blood cells (RBCs) during erythropoiesis in the bone marrow.
Heme Synthesis
- The iron part, also known as the heme part, is synthesized in the cytoplasm and mitochondria of developing RBC1.
- Haem synthesis occurs both in cytosol and in mitochondria of erythrocytes.
- Protoporphyrin is synthesized from the condensation of glycine and succinyl coenzyme A, eight molecules of each being required to form a linear tetrapyrrole molecule, which finally cyclizes into the protoporphyrin ring.
Globin Synthesis
The protein part, also known as the globin protein, is synthesized by the ribosome of the growing RBC.
Hemoglobin Assembly
- Each hemoglobin molecule is made up of four heme groups surrounding a globin group, forming a tetrahedral structure.
- Heme, which accounts for only 4 percent of the weight of the molecule, is composed of a ringlike organic compound known as a porphyrin to which an iron atom is attached.
- It is the iron atom that binds oxygen as the blood travels between the lungs and the tissues.
- There are four iron atoms in each molecule of hemoglobin, which accordingly can bind four molecules of oxygen.
- Globin consists of two linked pairs of polypeptide chains.
Release into Bloodstream
After a few days the cell loses its nucleus and is then introduced into the bloodstream in the vascular channels of the marrow.
Anaemia
Anemia is a condition that develops when your blood lacks enough healthy red blood cells or hemoglobin.
Symptoms
Symptoms of anemia may include fatigue, weakness, pale or yellowish skin, cold hands and feet, dizziness, and shortness of breath.
Causes
- Anemia can occur due to various reasons such as reduced production of red blood cells, excess blood loss, or destruction of the red blood cells.
- Conditions that may lead to anemia include heavy periods, pregnancy, ulcers, colon polyps or colon cancer, inherited disorders, a diet that does not have enough iron, folic acid or vitamin B12, blood disorders such as sickle cell anemia and thalassemia, or cancer.
Risk Factors
Risk factors include malnutrition, problems in absorption of nutrients due to conditions like Crohn’s disease or Celiac disease, excessive bleeding during menstruation, lack of balanced diet during pregnancy, and family history.
Complications
If untreated, anemia may lead to severe fatigue, complications in pregnancy, rapid or irregular heartbeat, and even heart failure.
Prevention
Anemia can be prevented by consuming a healthy diet rich in iron, Vitamin B12, and folic acid.
Diagnosis
Anemia is diagnosed with a physical exam and blood tests.
Treatment
Treatment for anemia might involve taking supplements, having medical procedures, or eating a healthy diet.
Mechanism of coagulation
Initiation
- Coagulation begins almost instantly after an injury to the endothelium that lines a blood vessel.
- Exposure of blood to the subendothelial space initiates two processes: changes in platelets, and the exposure of subendothelial platelet tissue factor to coagulation factor VII, which ultimately leads to cross-linked fibrin formation.
Extrinsic Pathway
- The extrinsic pathway is triggered by external trauma which causes blood to escape the circulation.
- Damage to the blood vessel means that factor VII exits the circulation into surrounding tissues.
- Tissue factor (factor III) is released by damaged cells outside the circulation.
- Factor VII and factor III form a complex, known as the TF-VIIa complex.
- TF-VIIa then activates factor X into its active form, factor Xa.
- In conjunction with factor Va, this triggers the formation of thrombin.
Intrinsic Pathway
- The intrinsic pathway is triggered by internal damage to the vessel wall.
- Factor XII is activated once it comes into contact with negatively charged collagen on the damaged endothelium.
- Along with clotting factors, platelets form a cellular ‘plug’ at the site of injury.
- These platelets also release mediators that facilitate further clotting, including Factor VIII.
- Factor IX combines with Factor VIII to form an enzyme complex that activates factor X, which along with factor Va, stimulates the production of thrombin.
Common Pathway
- The intrinsic and extrinsic pathways converge to give rise to the common pathway.
- The activated factor X causes a set of reactions resulting in the inactive enzyme prothrombin (also called factor II) being converted to its active form thrombin (factor IIa) by Prothrombinase.
- The thrombin then converts soluble fibrinogen (also referred to as factor I) into insoluble fibrin strands.
- The fibrin strands which comprise the clot are stabilised by factor XIII.
Regulation of Clotting
- To prevent excessive clotting and subsequent disease, mediators including Protein C and Protein S provide negative feedback on the clotting cascade.
- Protein C is activated following contact by thrombomodulin, which is itself activated by thrombin.
- Along with co-factors including protein S, activated protein C degrades factor Va and factor VIIIa, thus slowing the rate of clotting.
Blood grouping
Blood grouping is the classification of blood based on the presence or absence of specific antigens on the surface of red blood cells.
Antigens
- Antigens are substances that can trigger an immune response if they are foreign to the body.
- The presence or absence of these antigens determines a person’s blood type.
Major Blood Groups
- There are four major blood groups determined by the presence or absence of two antigens, A and B, on the surface of red blood cells.
- These groups are A, B, AB, and O.
Rh Factor
- In addition to the A and B antigens, there is a protein called the Rh factor, which can be either present (+) or absent (–).
- This creates the 8 most common blood types (A+, A-, B+, B-, O+, O-, AB+, AB-).
Blood Type Determination
- Blood types are inherited and represent contributions from both parents.
- An individual’s blood type is one of many possible combinations of blood-group antigens.
Blood Transfusion
- Safe blood transfusions depend on careful blood typing and cross-matching.
- The right blood transfusion can mean the difference between life and death.
- Also, Rh-negative blood is given to Rh-negative patients, and Rh-positive or Rh-negative blood may be given to Rh-positive patients.
- The universal red cell donor has Type O negative blood. The universal plasma donor has Type AB blood
| Blood Group | Blood Group | Antibodies |
| A | A | B |
| B | B | A |
| AB | A, B | None |
| O | None | A, B |
Blood Group A
- Has A antigens on the red cells.
- Has B antibodies in the plasma.
Blood Group B
- Has B antigens on the red cells.
- Has A antibodies in the plasma.
Blood Group AB
- Has both A and B antigens on the red cells.
- Does not have A or B antibodies in the plasma.
Blood Group O
- Does not have A or B antigens on the red cells.
- Has both A and B antibodies in the plasma.
Disorders of blood
Anemia
- Anemia is a condition that develops when your blood lacks enough healthy red blood cells or hemoglobin.
- Common types of anemia include iron-deficiency anemia, pernicious anemia, aplastic anemia, and hemolytic anemia.
Bleeding Disorders
- Bleeding disorders such as hemophilia and von Willebrand’s disease affect how your blood clots.
- These disorders can lead to excessive bleeding and bruising.
Blood Clotting Disorders
- Blood clotting disorders, also known as thrombophilia, affect your platelets or your clotting factors.
- These disorders can increase your risk of developing abnormal blood clots in your veins, such as deep vein thrombosis and pulmonary embolism.
Blood Cancers
- Blood cancers such as leukemia, lymphoma, and myeloma affect the production and function of your blood cells.
- Most of these cancers start in your bone marrow where blood is produced.
Platelet Disorders
- Platelet disorders affect your platelets and cause issues that may increase your risk of blood clots or make you bleed more than normal.
- Examples include thrombocytopenia and thrombocytosis.
Sickle Cell Disease
- Sickle cell disease is a group of disorders that affects hemoglobin, the molecule in red blood cells that delivers oxygen to cells throughout the body.
- People with this disorder have atypical hemoglobin molecules called hemoglobin S, which can distort red blood cells into a sickle, or crescent, shape.
Thalassemia
- Thalassemia is an inherited blood disorder that causes your body to have less hemoglobin than normal.
- This can lead to anemia.
Reticulo endothelial system
Definition
- The reticuloendothelial system (RES) is a network of cells and tissues found throughout the body, especially in the blood, general connective tissue, spleen, liver, lungs, bone marrow, and lymph nodes.
- It is a heterogeneous population of phagocytic cells in systemically fixed tissues that play an important role in the clearance of particles and soluble substances in the circulation and tissues.
History
- The term “reticuloendothelial system” (abbreviated RES) was employed by the beginning of the 20th century to denote a system of specialized cells that effectively clear colloidal vital stains from the blood circulation.
- The term is still used today, but its meaning has changed over the years, and is used inconsistently in present-day literature.
Composition
The composition of the reticuloendothelial system includes Kupffer cells of the liver, microglia of the brain, alveolar macrophages, bone marrow, lymph nodes, and macrophages in the intestine and other tissues.
Function
- The reticuloendothelial system plays an important role in the clearance of particles and soluble substances in the circulation and tissues.
- Substances that are cleared include immune complexes, bacteria, toxins, and exogenous antigens.
Regulation
- The reticuloendothelial system is also under the leading role of the nervous system and is regulated by chemicals in the body fluids.
- The state of the cerebral cortex has a great influence on the activity of macrophages in the reticuloendothelium.
Conclusion
Blood, the life-sustaining fluid, plays a crucial role in our body. It not only delivers essential nutrients and oxygen to our cells but also removes metabolic waste. The composition of blood, including red blood cells, white blood cells, and platelets, each serve unique and vital functions. The process of hematopoiesis and the formation of hemoglobin are complex yet essential for the proper functioning of our body. Disorders of blood, such as anemia and blood clotting disorders, can have significant impacts on health. The reticuloendothelial system and blood grouping further add to the complexity and functionality of blood. Understanding these aspects of blood is fundamental to appreciating its role in sustaining life. As we continue to explore the intricacies of blood, we uncover more about this vital fluid that silently courses through our veins, keeping us alive and healthy.
For more regular updates you can visit our social media accounts,
Instagram: Follow us
Facebook: Follow us
WhatsApp: Join us
Telegram: Join us
