Metformin Unveiled: A Scientific and Clinical Guide
Metformin is one of the most widely prescribed and well-studied oral antidiabetic medications in the world. Metformin, a first-line therapy for type 2 diabetes, has been in clinical use for decades due to its proven efficacy, safety profile, and additional benefits beyond blood sugar control. This comprehensive guide delves into the drug’s pharmacology, mechanism of action, therapeutic uses, side effects, contraindications, and emerging research. Whether you are a healthcare professional, pharmacy student, or researcher, this article provides an in-depth scientific and clinical understanding of metformin, helping you appreciate its pivotal role in diabetes management and beyond.
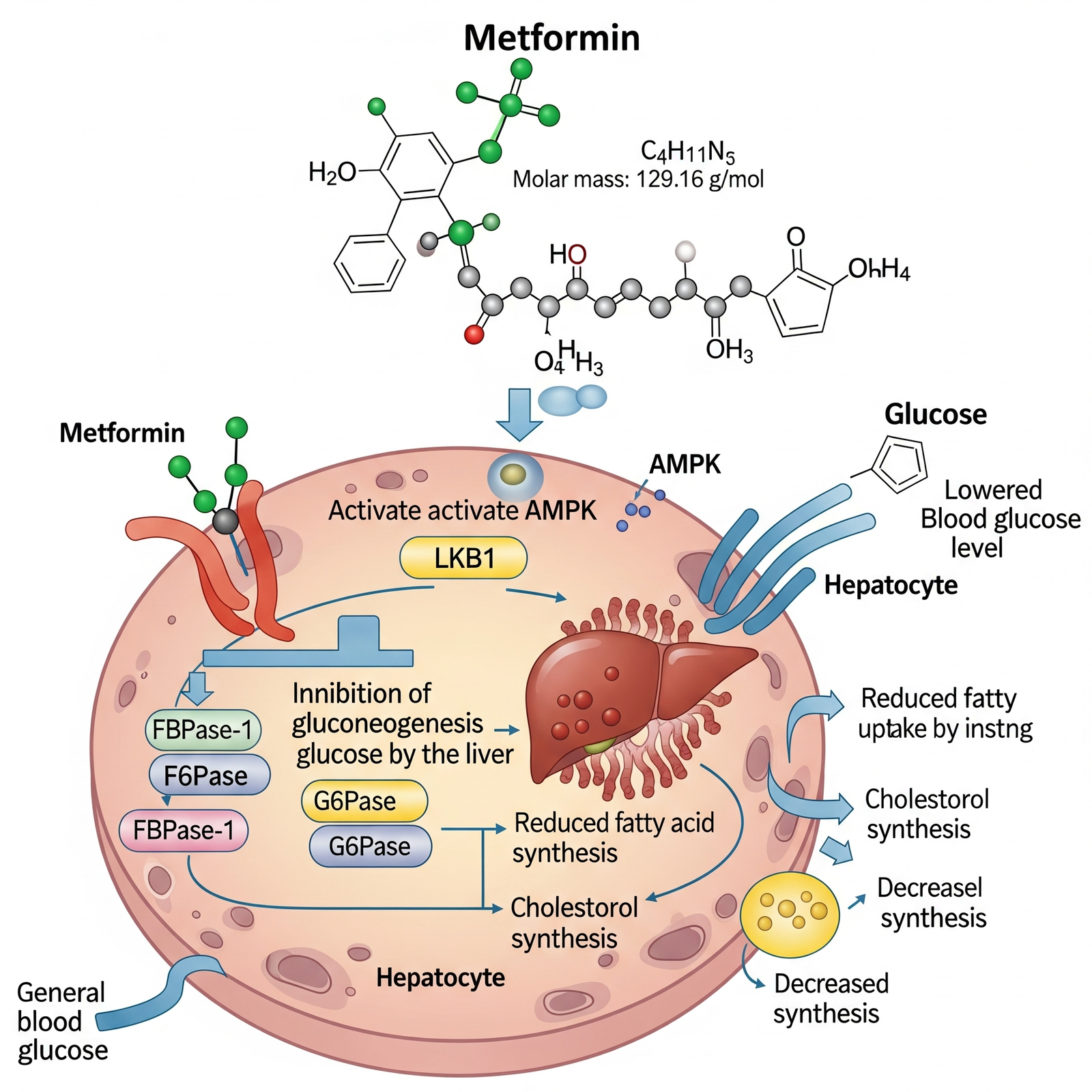
1. Chemical Structure and Medicinal Chemistry (In-Depth)
- Chemical Class: Biguanide
- IUPAC Name: 1,1-Dimethylbiguanide
- CAS Number: 657-24-9
- Molecular Formula: C₄H₁₁N₅
- Structure:
- Two guanidine groups connected by a nitrogen-carbon-nitrogen backbone
- Terminal dimethyl groups improve solubility and stability
Physicochemical Properties:
- Highly hydrophilic and zwitterionic at physiological pH
- Lacks lipid solubility → Low membrane permeability
- pKa: ~12.4 → Ionized at body pH
- LogP: -1.43 → Poor lipophilicity
Medicinal Chemistry Relevance:
- Not metabolized by liver enzymes, unlike most oral antidiabetics
- Depends on organic cation transporters (OCTs) for cell entry:
- OCT1: Expressed in hepatocytes (critical for hepatic action)
- OCT2: Renal tubular secretion
- MATE1/MATE2-K: Eliminate metformin into urine
- Structural simplicity provides low drug-drug interaction potential at the CYP level but important interactions at transporter level
2. Pharmacological Classification (Expanded)
| Property | Detail |
|---|---|
| Drug Class | Biguanides (others like phenformin were withdrawn due to lactic acidosis) |
| Therapeutic Category | Oral antihyperglycemic agent |
| ATC Code | A10BA02 |
| Mechanism Group | Insulin sensitizer |
Unique Pharmacologic Characteristics:
- Does not act on pancreatic β-cells
- Minimal to no hypoglycemia in monotherapy
- Associated with weight neutrality or modest loss
- Strong cardiometabolic benefit, as shown in the UKPDS trial
3. Mechanism of Action (In-Depth)
Metformin’s mechanism is multifactorial, involving cellular energy metabolism, signaling pathways, and hormonal modulation:
A. Primary Mechanism – Suppression of Hepatic Gluconeogenesis
- Inhibits mitochondrial respiratory-chain complex I → ↓ ATP, ↑ AMP/ATP ratio
- Energy depletion activates AMPK (adenosine monophosphate-activated protein kinase)
B. AMPK Activation Effects
- ↓ Expression of gluconeogenic genes (PEPCK, G6Pase)
- ↑ Fatty acid oxidation
- ↓ Lipogenesis via inhibition of ACC (acetyl-CoA carboxylase)
- ↓ Hepatic glucose output
C. Inhibition of Glucagon Signaling
- ↓ cAMP production in hepatocytes by inhibiting adenylate cyclase
- ↓ Glucagon-mediated gluconeogenesis
D. Gut-Based Mechanism
- Enhanced GLP-1 secretion
- Delayed glucose absorption from intestinal lumen
- Increased lactate production by enterocytes → may explain rare lactic acidosis
E. Microbiome Modulation
- Promotes short-chain fatty acid production
- Increases abundance of Akkermansia muciniphila, improving insulin sensitivity
4. Pharmacokinetics (More Detailed)
| Parameter | Value |
|---|---|
| Oral Bioavailability | 50–60% (decreases with higher doses) |
| Time to Peak | 1–3 hrs (IR), ~7 hrs (XR) |
| Distribution Volume | 654 ± 358 L (high tissue binding, especially in GI tract) |
| Plasma Protein Binding | <5% |
| Half-Life | 4–6 hrs (plasma), 20 hrs (GI mucosa) |
| Metabolism | None |
| Excretion | 100% unchanged in urine (via tubular secretion) |
Transporters Involved:
- OCT1: Hepatic uptake
- OCT2: Renal uptake from blood into tubular cells
- MATE1/2-K: Efflux into urine
Clinical Importance: Any genetic polymorphism or drug that inhibits these transporters (e.g. cimetidine, dolutegravir) can increase metformin levels → higher risk of lactic acidosis.
5. Therapeutic Uses (Expanded)
A. Type 2 Diabetes Mellitus (T2DM)
- First-line therapy (ADA, EASD, AACE guidelines)
- Effective for both fasting and postprandial glucose control
- Used in combination with SGLT2i, DPP-4 inhibitors, GLP-1 agonists, or insulin
B. Cardiovascular Protection
- UKPDS trial: Metformin reduced macrovascular complications in overweight patients
- Associated with lower MI and stroke risk
C. Polycystic Ovary Syndrome (PCOS)
- Improves hyperinsulinemia and ovulatory function
- Often used adjunctively with clomiphene in fertility treatment
D. Prediabetes
- DPP Trial: 31% relative risk reduction in progression to diabetes
- Especially beneficial in patients <60 years with BMI >35
E. Gestational Diabetes Mellitus (GDM)
- Evidence supports non-inferiority to insulin
- Safer profile and less maternal weight gain
F. Non-Alcoholic Steatohepatitis (NASH)
- AMPK activation helps reduce hepatic fat accumulation and inflammation
G. Cancer Prevention (Emerging Evidence)
- Reduced incidence of colon, pancreatic, and breast cancers via:
- AMPK activation
- mTOR inhibition
- Insulin/IGF-1 axis modulation
6. Dosage and Administration (Expanded)
Immediate-Release (IR):
- Start: 500 mg BID with meals
- Titrate weekly by 500 mg
- Max: 2550 mg/day (in divided doses)
Extended-Release (XR):
- Start: 500 mg or 750 mg QD with evening meal
- Titrate by 500 mg weekly
- Max: 2000 mg/day
Renal Function-Based Dosing:
| eGFR (mL/min/1.73m²) | Use Recommendation |
|---|---|
| ≥60 | Full dose |
| 45–59 | Reduce dose, monitor renal function every 3–6 months |
| 30–44 | Do not initiate; if already on, reduce dose by 50% |
| <30 | Contraindicated |
7. Side Effects (Expanded with Mechanisms)
Gastrointestinal:
- Due to local action in enterocytes and serotonin release in GI tract
- Diarrhea, flatulence, nausea → resolve with time or XR form
Vitamin B12 Deficiency:
- Metformin interferes with calcium-dependent membrane action in ileum
- May lead to megaloblastic anemia, neuropathy
Lactic Acidosis:
- Rare but serious; due to impaired lactate clearance or increased production
- Associated with hypoxia, renal impairment, sepsis, or alcoholism
Dermatological:
- Rash, urticaria, or rare angioedema
8. Contraindications (Detailed)
- eGFR <30 or unstable renal function
- Acute conditions predisposing to hypoxia (heart failure, sepsis, dehydration)
- Recent surgery or contrast studies with iodinated media
- Severe liver disease
- Alcohol use disorder
Precautions:
- Temporarily withhold during acute illness, surgery, or radiologic studies
- Resume once renal function stabilizes
9. Drug Interactions (Detailed)
| Drug | Interaction |
|---|---|
| Cimetidine | Competes for OCT2, raises plasma metformin |
| Iodinated contrast | Risk of renal injury → lactic acidosis |
| Alcohol | Inhibits gluconeogenesis, increasing acidosis risk |
| Ranolazine, Dolutegravir, Trimethoprim | Inhibit MATE transporters |
| Steroids, Diuretics | Raise blood glucose, oppose metformin’s action |
10. Special Populations (Expanded)
Pregnancy:
- Safe and effective for GDM
- Crosses placenta, but no teratogenicity observed
- Lower maternal weight gain compared to insulin
Lactation:
- Very low levels in breast milk
- No adverse effects reported in infants
Elderly:
- Renal clearance declines → increased risk of lactic acidosis
- Monitor renal function every 3 months
11. Overdose and Toxicity (Expanded)
Clinical Presentation:
- Early: Nausea, vomiting, malaise
- Later: Hypothermia, hypotension, bradyarrhythmias, severe lactic acidosis
Investigations:
- Arterial blood gas: pH <7.2, elevated lactate >5 mmol/L
- Serum creatinine
- Plasma metformin level (not widely available)
Management:
- Immediate discontinuation
- Hemodialysis: Removes both metformin and corrects acidosis
- IV fluids, bicarbonate if pH <7.0
12. Brand Names
| Region | Common Brands |
|---|---|
| India | Glycomet, Obimet, Gluformin |
| US | Glucophage, Fortamet, Riomet |
| UK | Sukkarto, Glucient |
13. Clinical Pearls
- XR formulation improves adherence and GI tolerability
- Metformin is safe, cheap, and evidence-rich
- Always re-evaluate renal function periodically
- Educate patients about symptoms of B12 deficiency and lactic acidosis
- Combine with GLP-1 RAs or SGLT2i for synergistic effect
✅ Conclusion
Metformin remains one of the most widely prescribed and trusted oral antidiabetic drugs worldwide. Its unique mechanism of action—reducing hepatic glucose production, improving insulin sensitivity, and enhancing peripheral glucose uptake—makes it the first-line therapy in type 2 diabetes management. Beyond diabetes, metformin shows promising benefits in conditions like PCOS, obesity, and even in reducing cardiovascular risk. Despite its safety profile, healthcare professionals must consider contraindications such as renal or hepatic impairment and monitor patients for side effects like gastrointestinal disturbances and rare lactic acidosis. With ongoing research, metformin continues to demonstrate potential beyond glycemic control, reinforcing its role as a cornerstone in modern medicine.
❓ FAQs on Metformin
1. What is Metformin primarily used for?
Metformin is primarily prescribed for the management of type 2 diabetes mellitus. It helps lower blood sugar levels by reducing hepatic glucose production, enhancing insulin sensitivity, and improving glucose uptake in muscle tissues.
2. Can Metformin be used for conditions other than diabetes?
Yes. Apart from type 2 diabetes, metformin is also used in managing polycystic ovary syndrome (PCOS), obesity-related insulin resistance, and is being studied for its potential role in anti-aging, cardiovascular health, and cancer prevention.
3. What are the common side effects of Metformin?
The most common side effects include gastrointestinal issues such as nausea, diarrhea, abdominal discomfort, and bloating. These usually improve over time or with gradual dose titration. A rare but serious side effect is lactic acidosis, which requires immediate medical attention.
4. Who should avoid taking Metformin?
Metformin should be avoided in individuals with severe renal impairment, liver disease, alcohol abuse, or conditions predisposing to hypoxia (e.g., heart failure, severe infections). It is also contraindicated in patients undergoing contrast radiology procedures due to the risk of kidney injury.
5. When is the best time to take Metformin?
Metformin is best taken with meals to reduce gastrointestinal side effects. Depending on the formulation:
-
Immediate-release tablets are usually taken 2–3 times daily with meals.
-
Extended-release tablets are taken once daily, usually with the evening meal.
For more regular updates you can visit our social media accounts,
Instagram: Follow us
Facebook: Follow us
WhatsApp: Join us
Telegram: Join us